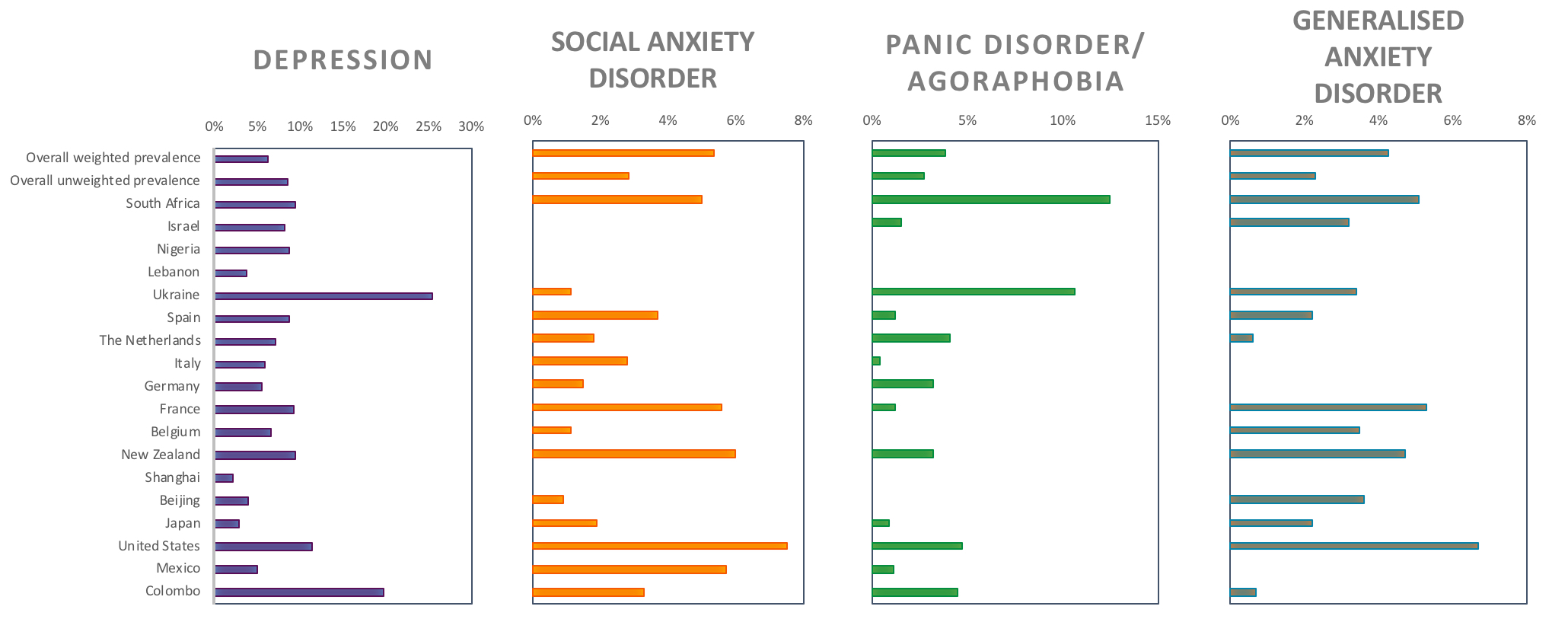
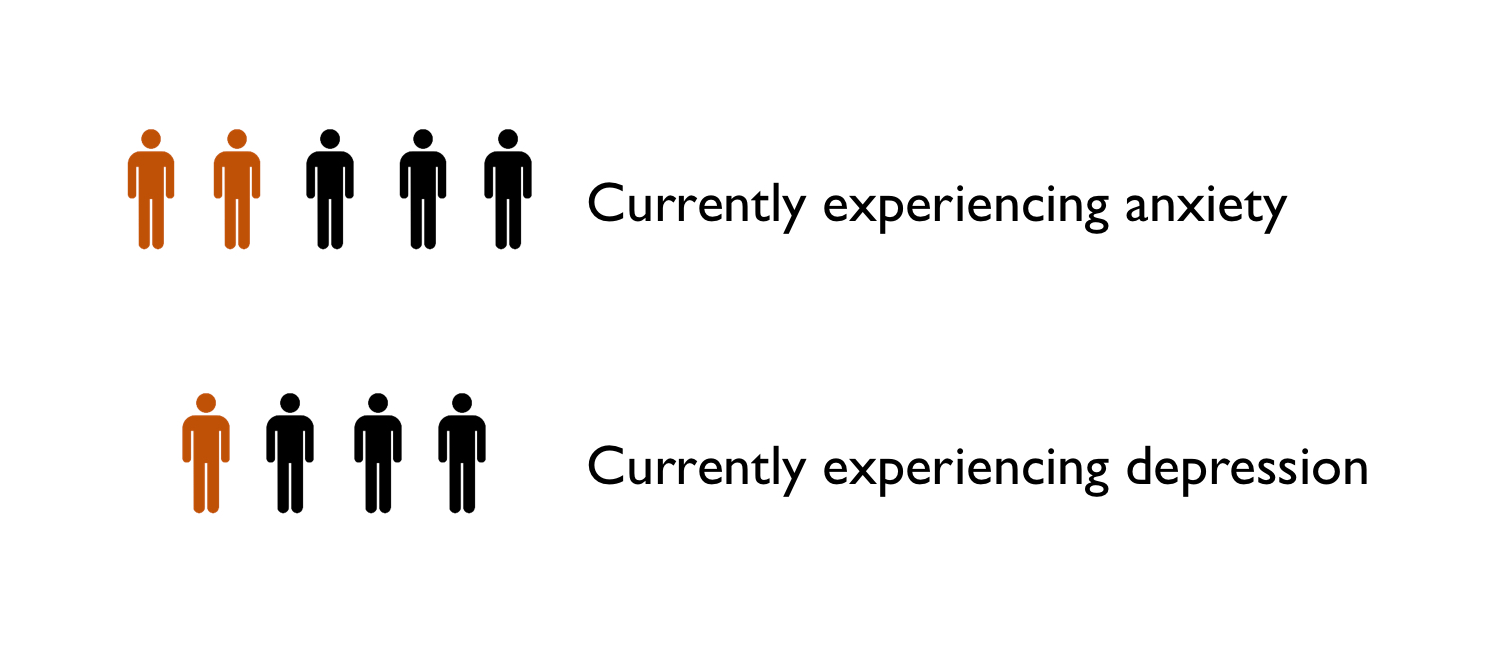
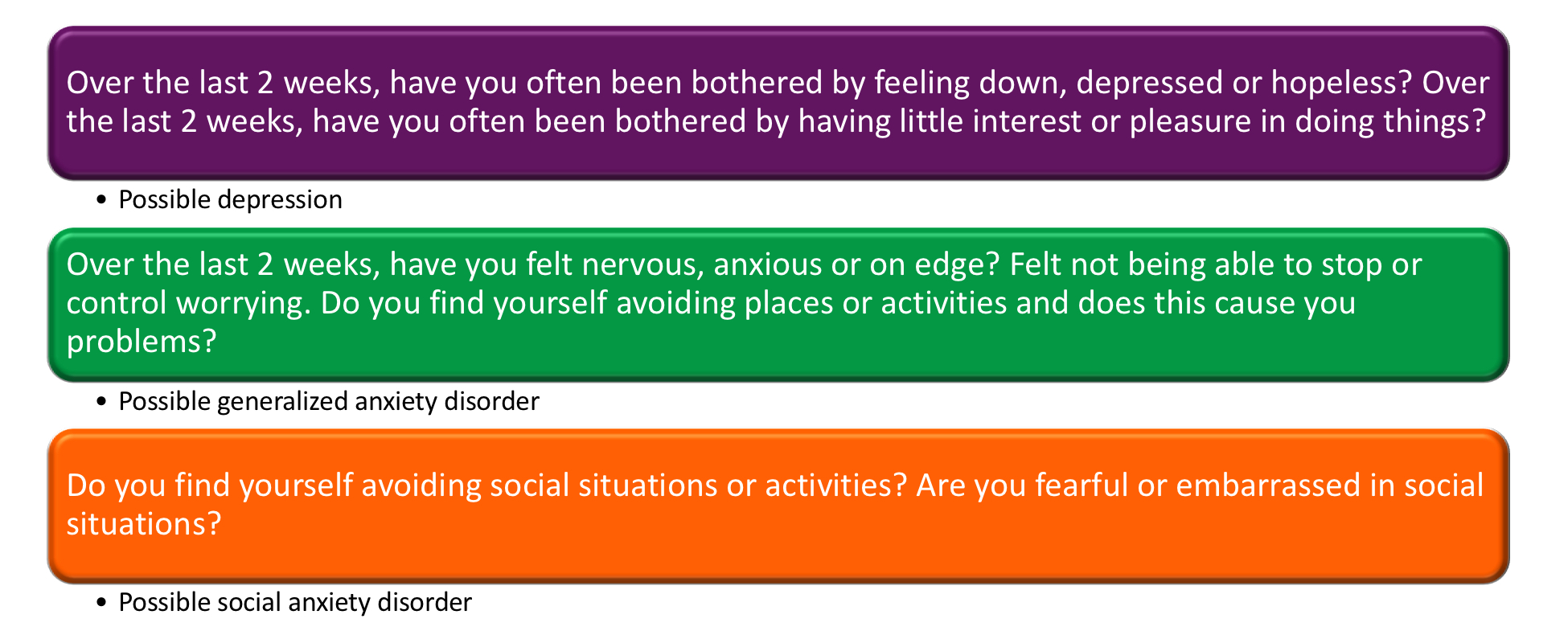
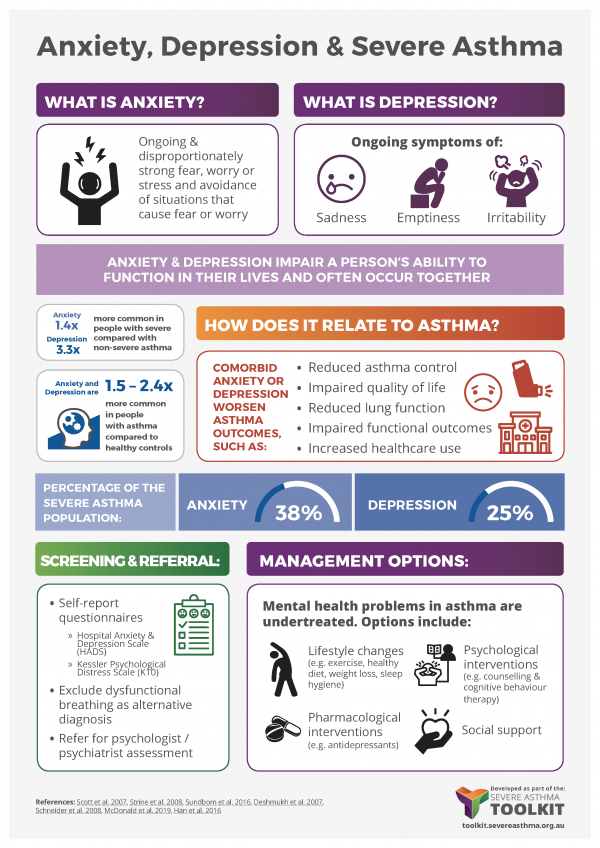
Anxiety and depression are two common mental health problems.
Anxiety involves ongoing and disproportionately strong feelings of fear, worry or stress, which can happen out of the blue or in response to particular situations or objects. It also involves avoiding situations and objects that may cause fear or worry.