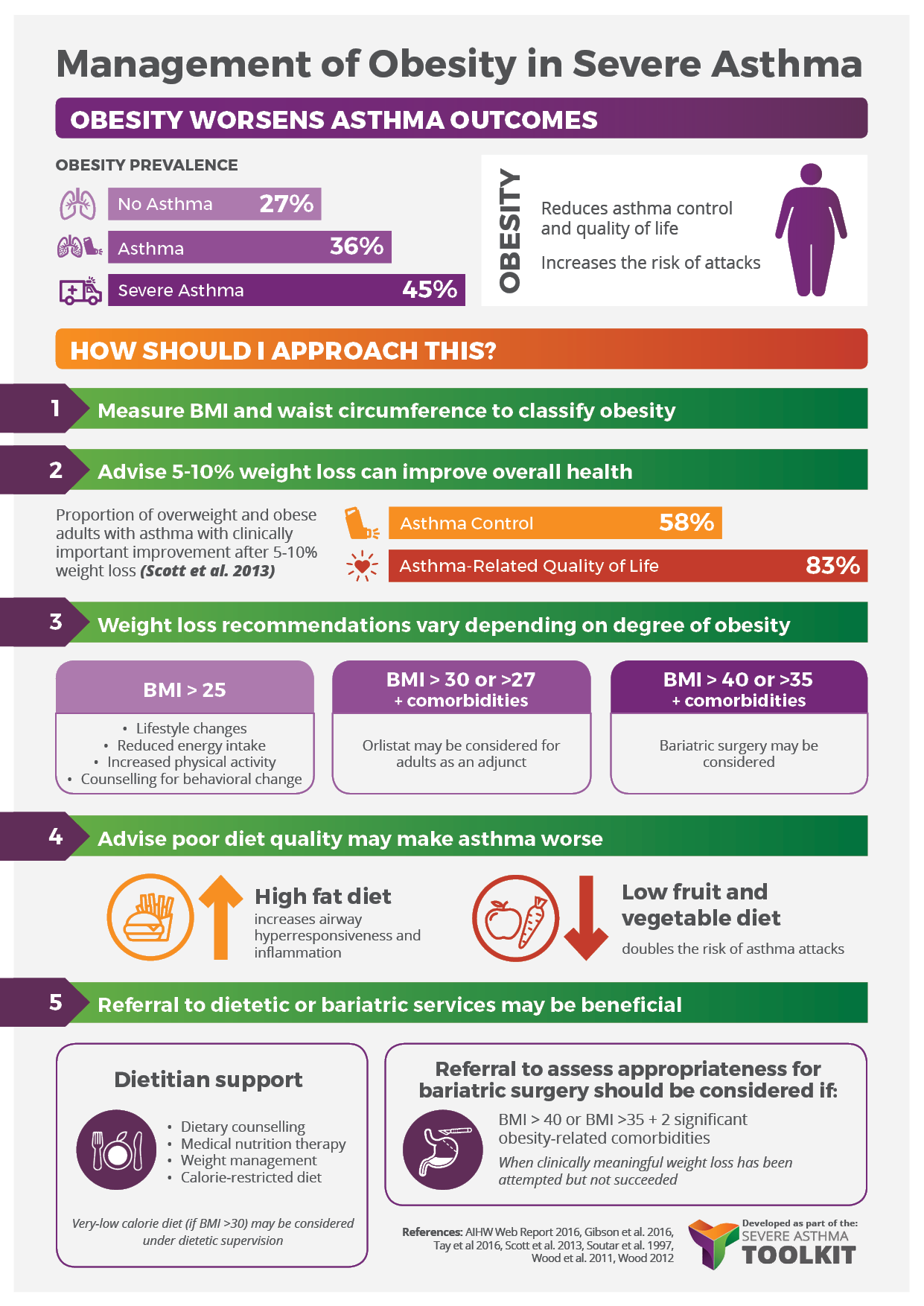
Asthma and Obesity
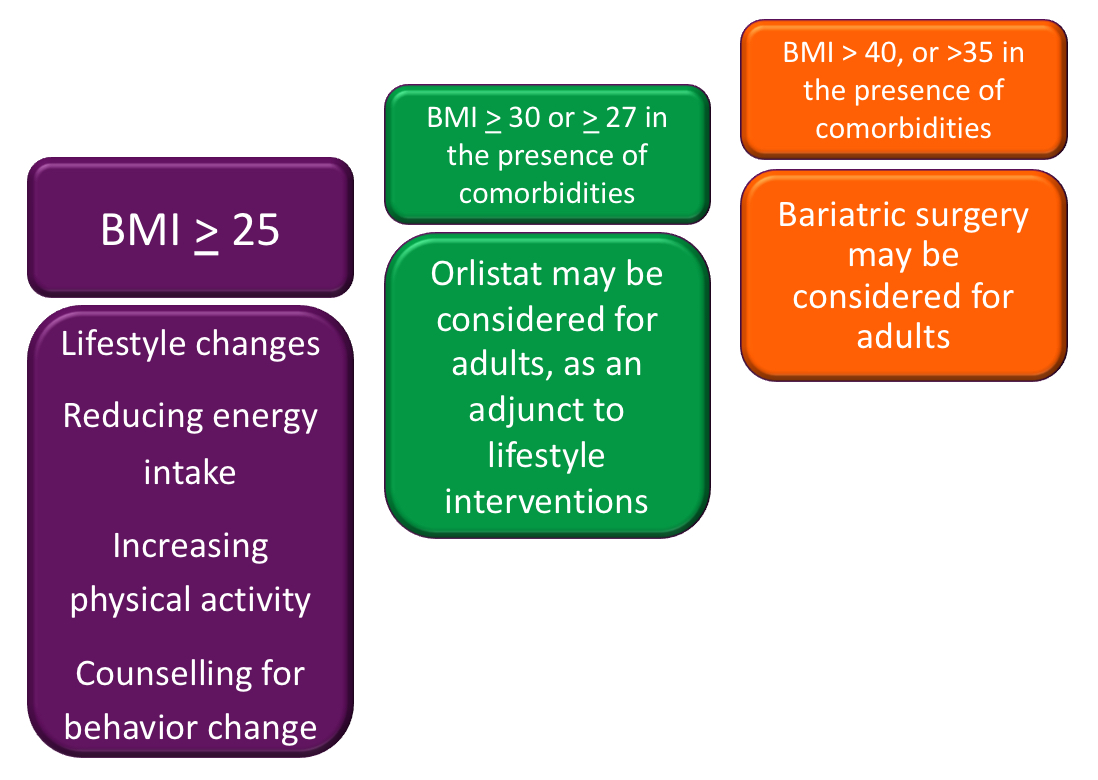
Obesity is a progressive and relapsing condition characterised by abnormal or excessive accumulation of fat and is becoming increasingly common. Obesity is associated with increased risk of non-communicable disease and is preventable.