Asthma Self-Monitoring
Establish the patient’s preference to use symptoms or peak expiratory flow to monitor severe asthma.
Establish the patient’s preference to use symptoms or peak expiratory flow to monitor severe asthma.
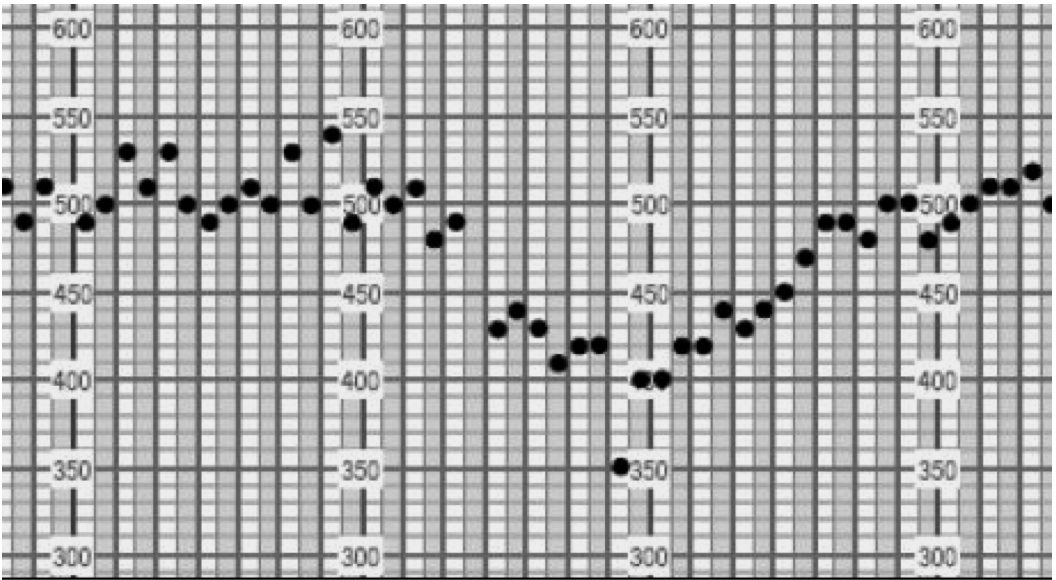
An example of an asthma flare-up on a compressed PEF chart.
Last Updated on