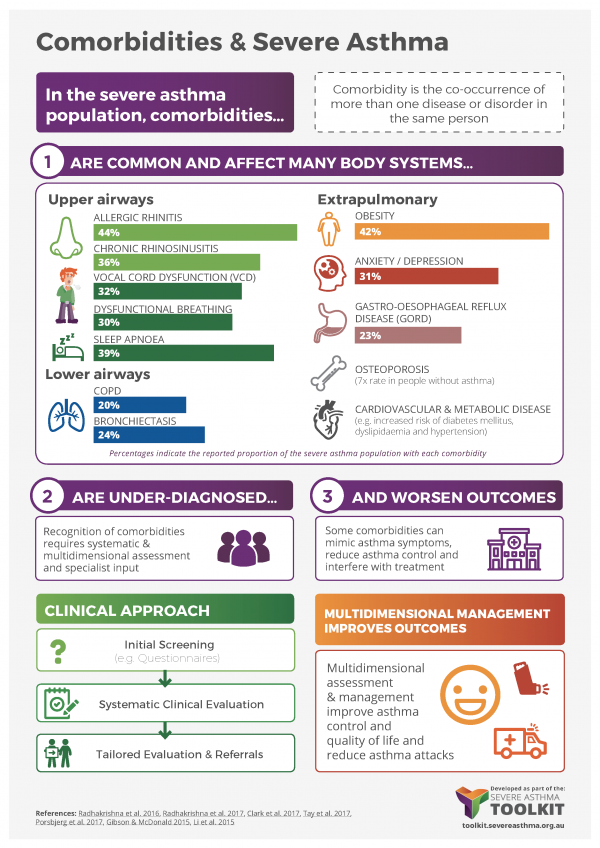
Comorbidities in severe asthma are common, they complicate management and effect patient outcome. Comorbidities may frequently interact, contribute to poor disease control and mimic symptoms of asthma. They may also increase the cost of treatment for people with severe asthma and lead to overtreatment. It is therefore recommended that comorbidities be addressed in severe asthma (Chung et al. 2014). Multidimensional assessment of severe asthma allows for the recognition of these comorbidities and has been shown to improve patient outcomes (Clark et al. 2017). In this module, we deal with the most common comorbidities associated with severe asthma, we present their prevalence and impact and provide recommendations for assessment and management.
LAY OVERVIEW
People with severe asthma often have other medical problems. These comorbidities can make a person’s asthma worse and more difficult and expensive to manage and treat. People may end up taking too many medications. When people have a multidimensional assessment of severe asthma, their other medical problems and treatments are taken into account and this improves asthma outcomes.
Comorbidities are Common
Many comorbidities are more prevalent in people with severe asthma than in mild-moderate asthma, or in the healthy population. Their prevalence in a difficult-to-treat asthma cohort (most of whom had severe asthma) is shown below.
- Percentage of patients
Comorbidities Are Under-Diagnosed
While respiratory physicians are adept at recognising some comorbidities (such as obstructive sleep apnoea, bronchiectasis and COPD), others often go undiagnosed even in specialist practice (such as dysfunctional breathing and vocal cord dysfunction) (Radhakrishna et al. 2017).
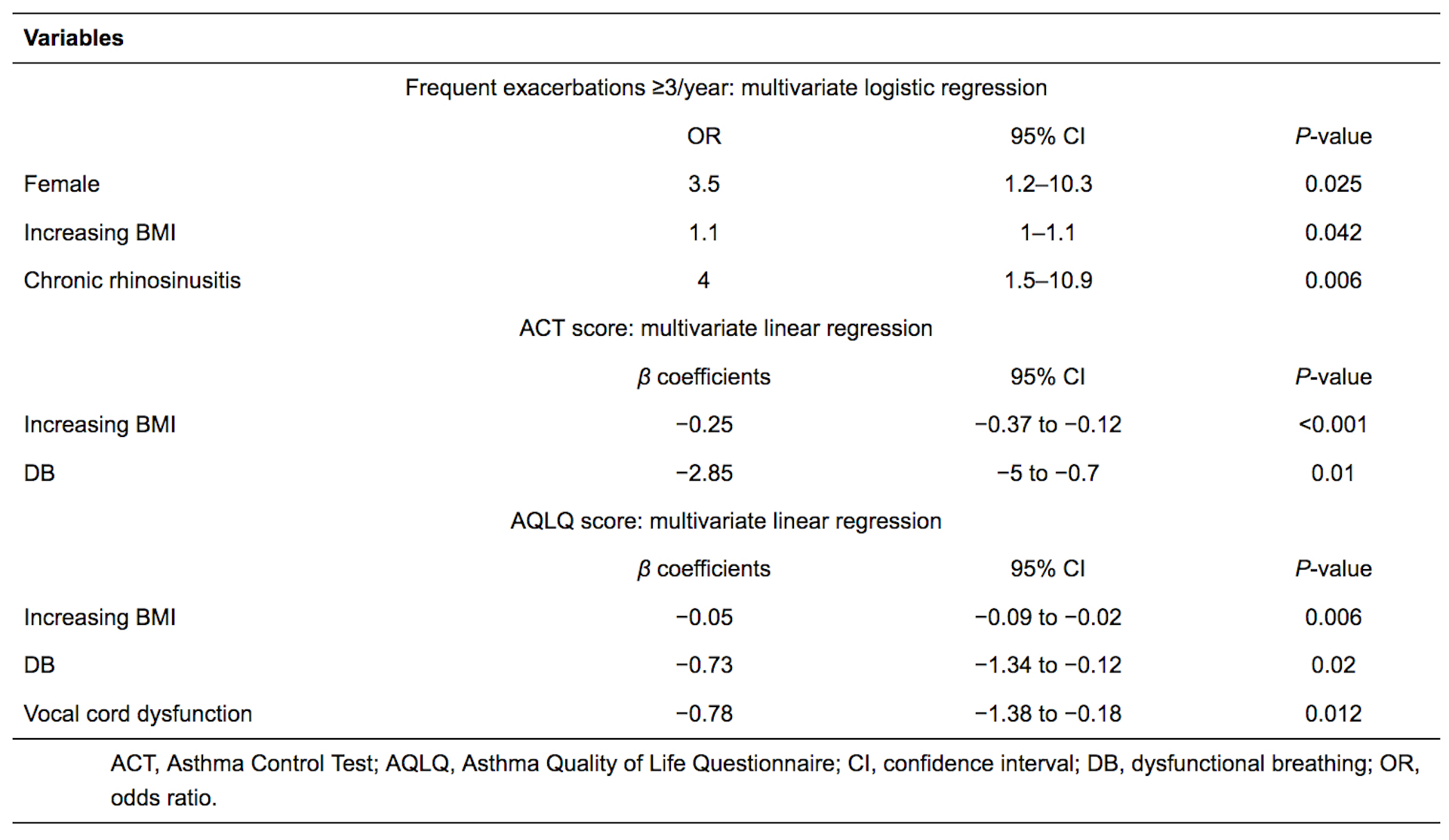
Comorbidities Worsen Asthma Outcomes
There is data to indicate that the presence of comorbidities is associated with worse asthma outcomes for patients. For example, the presence of chronic rhinosinusitis is a strong risk factor for frequent exacerbations (ten Brinke et al. 2005, Tay et al. 2016, Denlinger et al. 2017). Other risk factors for exacerbations, poor asthma control, and impaired quality of life include gender, body mass, dysfunctional breathing and vocal cord dysfunction (Tay et al. 2016).
Treatment of Comorbidities Is Associated with Improved Asthma Outcomes
Based mainly on observational studies, treatment of many comorbidities appears to improve asthma outcomes (Porsbjerg et al. 2017, Tay et al. 2017).
Clinical approaches to severe asthma comorbidities
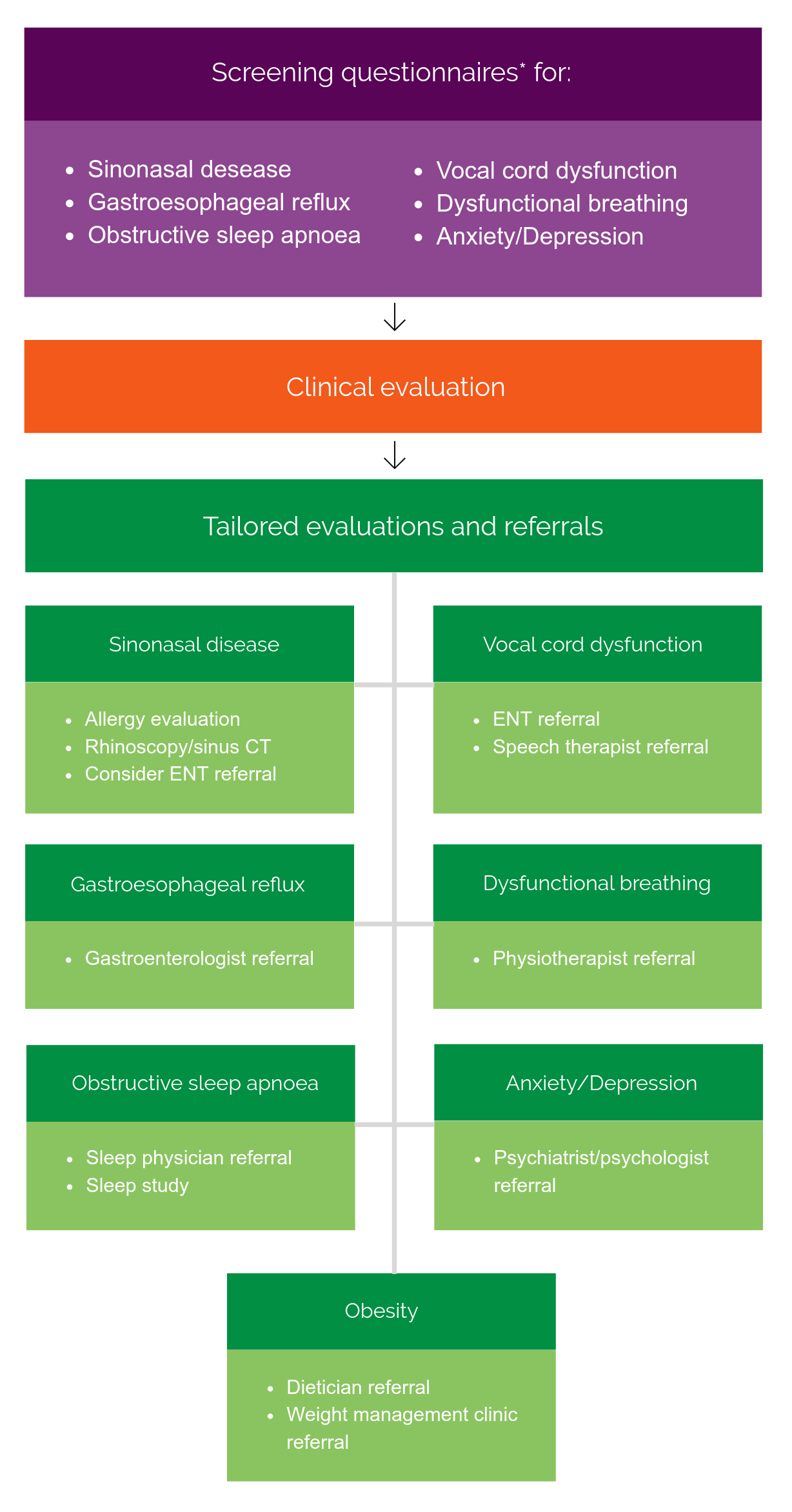
The multitude of patient comorbidities to be considered during severe asthma evaluation presents a clinical challenge. An unstructured approach is likely to miss several issues. On the other hand, exhaustive evaluation with every possible diagnostic test would be costly in resources and time. A third option is to employ a stratified approach, shown below.
This commences with the use of validated screening questionnaires for each comorbidity. An overview of validated screening tools is included below. As an example, the following scored and validated questionnaires and there sensitivity / specificity are proposed for screening by (Radhakrishna et al. 2017)
- Sinonasal Questionnaire (SNQ) for sino-nasal disease
- Score for Allergic Rhinitis (SFAR) for allergic rhinitis
- Nijmegen Questionnaire for dysfunctional breathing
- Pittsburgh Vocal Cord Dysfunction Index (PVCDI) for vocal cord dysfunction
- Berlin Questionnaire for obstructive sleep apnoea
- Hospital Anxiety and Depression Scale (HADS) for anxiety & depression
- Gastroesophageal Reflux Disease Questionnaire (GERD-Q) for gastro-oesophageal reflux disease
For further details see the Comorbidity Components Resources section of this website.
Such an approach has been shown to increase detection of comorbidities compared to clinical consultation alone (Radhakrishna et al. 2017). Positive questionnaires guide the clinician to confirm the likelihood of comorbidities being present, and prompt appropriate further management.
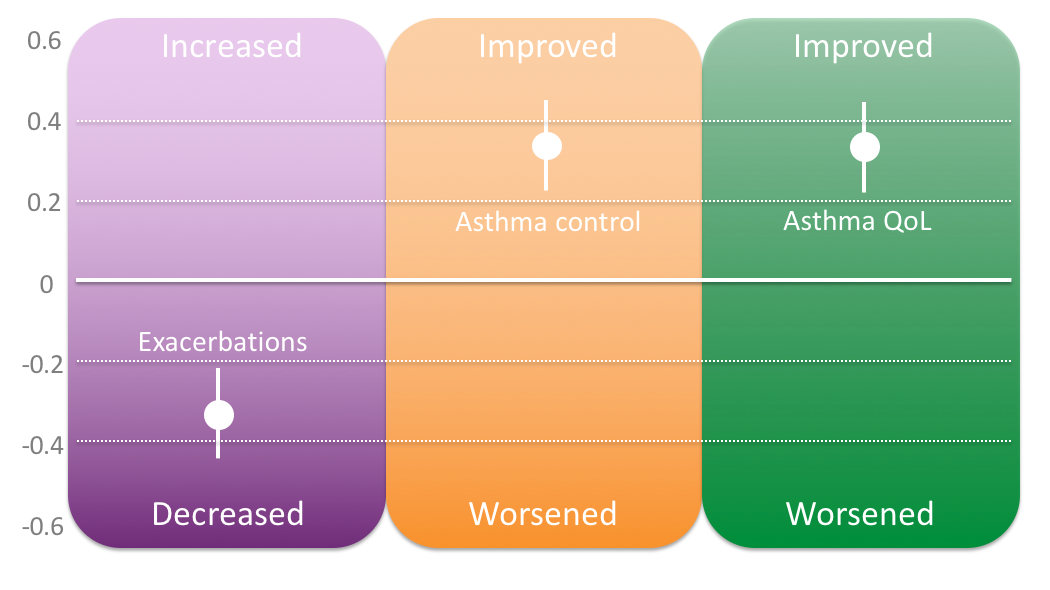
A systematic approach to addressing severe asthma comorbidities in patients is clinically effective. A recent meta-analysis of three severe asthma programs which addressed comorbidities systematically as part of their protocol demonstrated improvements in asthma control, asthma quality of life and exacerbation rate (Clark et al. 2017).
- Allergic & Non-Allergic Rhinitis
- Chronic Rhinosinusitis
- Dysfunctional Breathing
- Vocal Cord Dysfunction
- Chronic Obstructive Pulmonary Disease
- Bronchiectasis
- Obstructive Sleep Apnoea
- Obesity
- Anxiety & Depression
- Gastro-oesophageal Reflux Disease (GORD)
- Osteoporosis
- Cardiovascular Disease & Metabolic Disease
Last Updated on