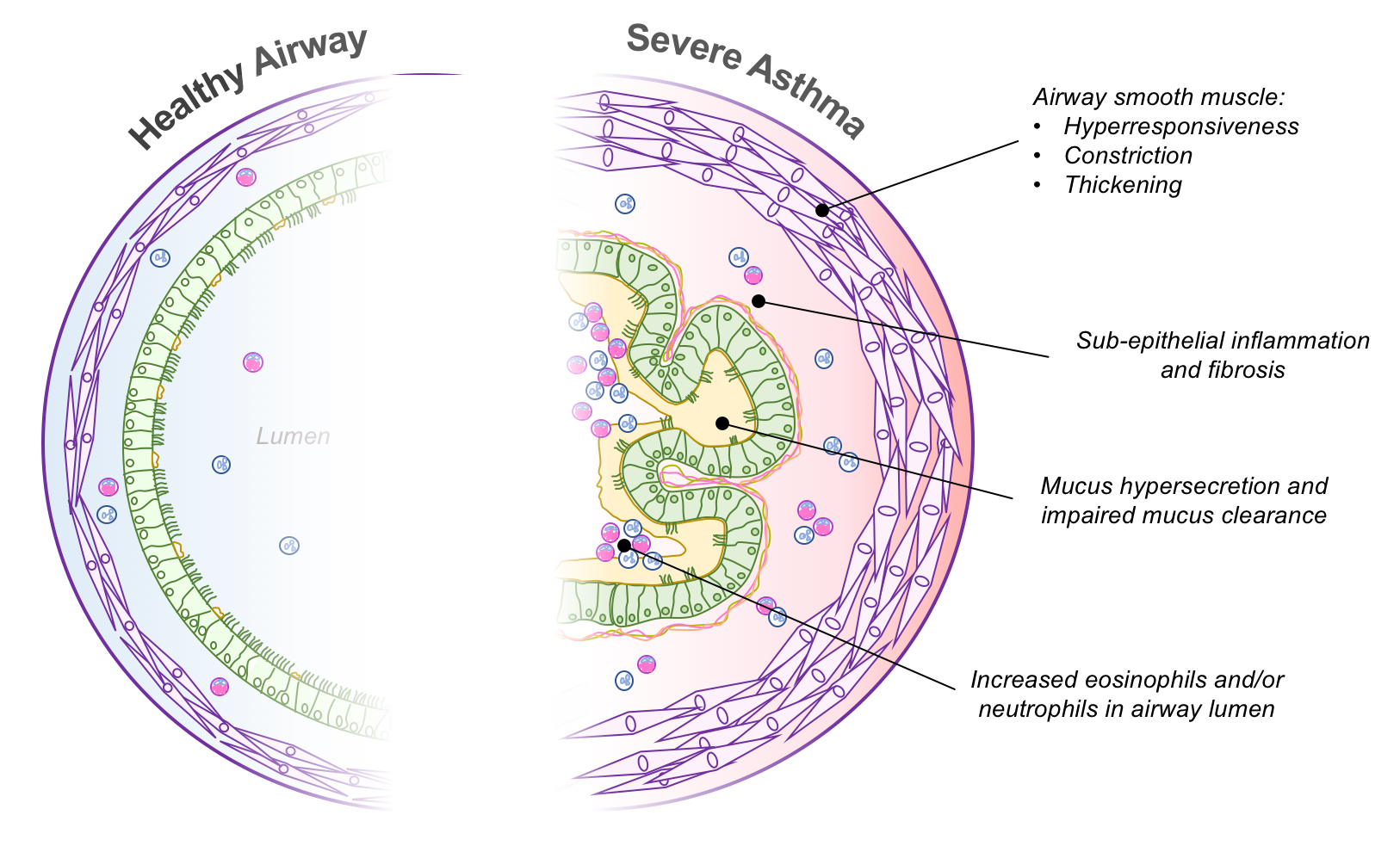
The development of asthma and resulting asthma severity are governed by complex interactions between genetic and environmental factors. The key pathophysiological features of asthma pathology are lung inflammation, airway hyper-responsiveness, airway remodelling and mucous hypersecretion, all of which contribute to variable airflow limitation. Importantly, it is increasingly recognised that asthma is not a single or homogenous disease, but is better thought of as a condition that may arise as a combination of variations of the key pathophysiological features described above (Trejo Bittar et al. 2015, Israel et al. 2017).
Severe asthma is certainly no different in this respect; indeed, the recognition and measurement of this pathophysiological heterogeneity is increasingly important in terms of determining effective personalized treatment.