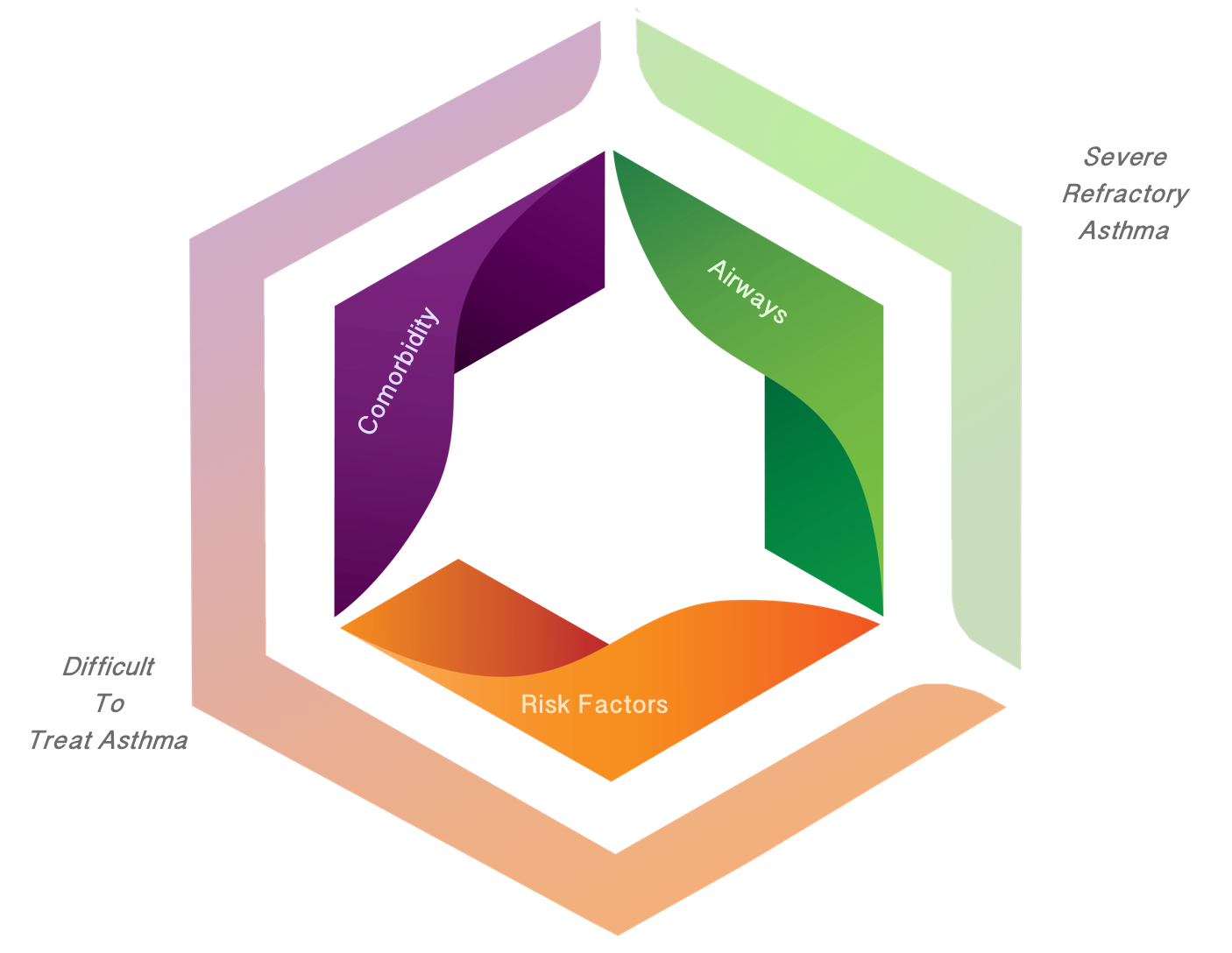
Severe Asthma Definition
Following confirmation of a diagnosis of asthma and after comorbidities have been addressed, severe asthma is defined as ‘‘asthma which requires treatment with high dose inhaled corticosteroids (ICS) plus a second controller (and/or systemic corticosteroids) to prevent it from becoming ‘uncontrolled’ or which remains ‘uncontrolled’ despite this therapy.’’ – (Chung et al. 2014)