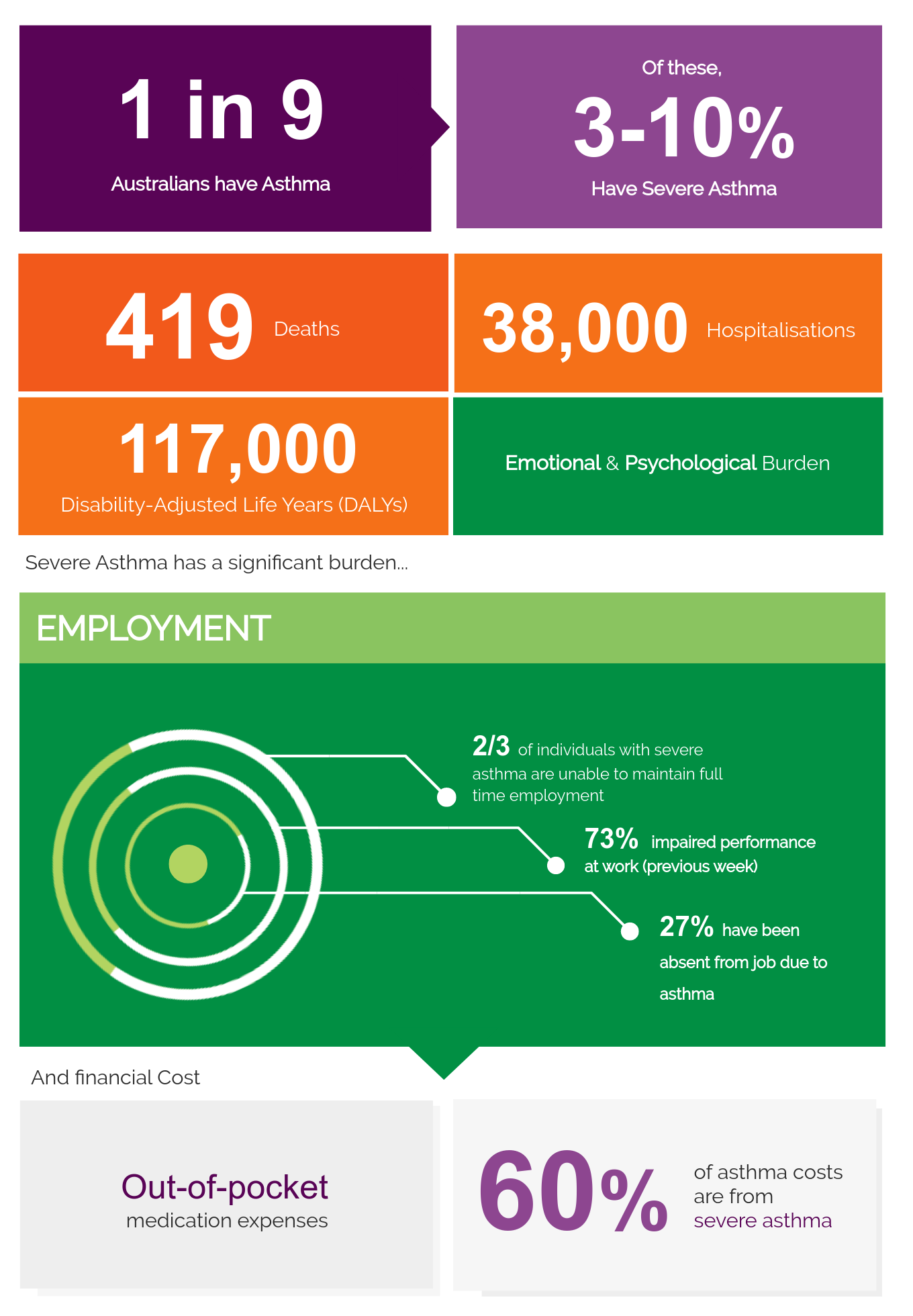
An estimated 1 in 9 Australians have asthma, which is approximately 2.7 million people, based on self-report (AIHW 2020). This is high by international standards. An estimated 300 million people have asthma worldwide.
Indigenous Australians are nearly twice as likely to report having asthma, compared to non-Indigenous populations (AIHW 2020).