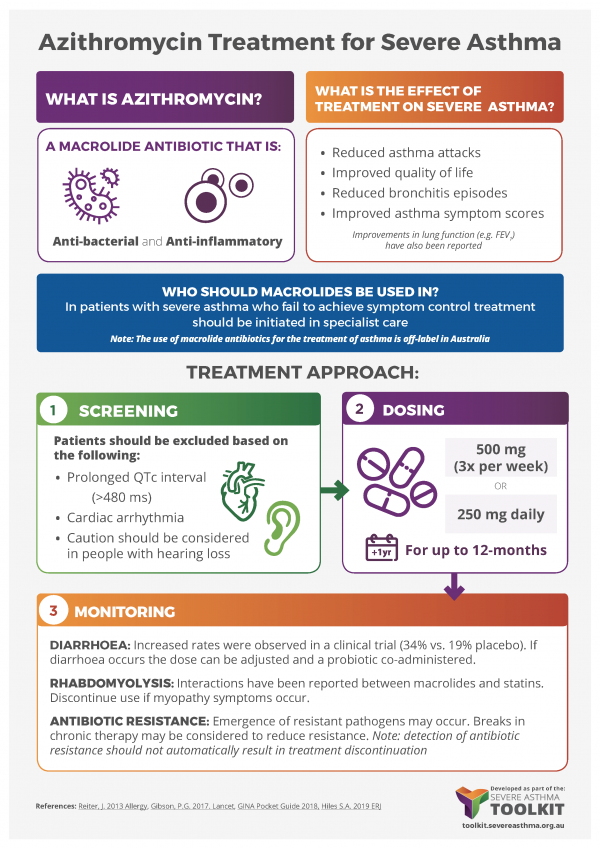
Add-on Therapy Symptom Control
Add-on therapies can be considered to improve symptom control or as a dose-reduction strategy to limit the side effects of primary therapies (e.g. high-dose corticosteroids or long-term oral corticosteroids). The biological processes underlying asthma are heterogeneous, so detailed characterisation of the individual patient phenotype and an individual risk/benefit assessment should be undertaken before proceeding with add-on therapies. For more information see Phenotypes & Phenotyping.
These can be trialled in individual patients by comparing symptom control before and after treatment for a defined period, at a time when nothing else is being changed (modified “n of 1 trials”). There is little point in continuing add-on therapies long term if there is no obvious improvement.