Written Asthma Action Plans
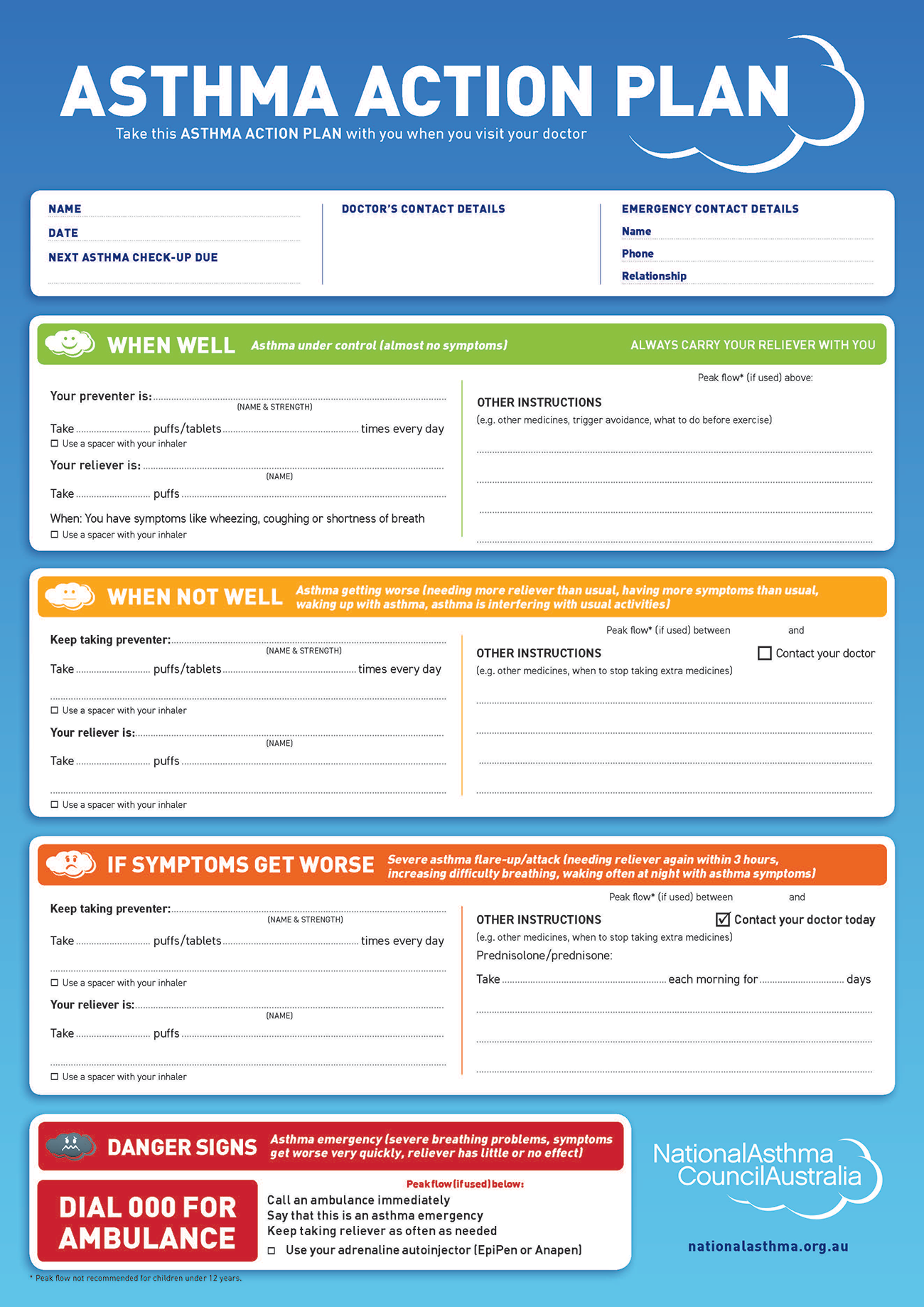
Personalised written asthma action plans show patients how to make short term changes to their treatment in response to changes in their symptoms or PEF. They also describe how and when to access medical care.
- Discuss the benefits of having and using a written Asthma Action Plan (AAP) with the patient, including: fewer attacks, doctor visits, hospitalisations and time off work. This evidence comes from general populations with mild to moderate asthma, not patients with severe asthma. (Gibson et al. 2004)
Increasing treatment in severe asthma when there is a worsening of symptoms or a decrease in PEF:
- Because patients are already taking maximum doses of inhaled medications, they should start a course of oral corticosteroids tablets for 10 days or return to their maximum dose if already on low dose oral corticosteroids. Encourage patients to continue to take all their prescribed inhalers and other severe asthma medications.
- If patients do not improve with oral corticosteroids or their symptoms worsen despite taking them, they usually need urgent medical/hospital treatment.